A mammogram is an imaging test that uses X-rays of the breasts to look for and identify breast cancer. The pictures are reviewed by a radiologist—a medical professional who specializes in evaluating imaging tests—to check for lumps, masses (tumors), changes in breast size or shape, and other signs of cancer. In general, your doctor could recommend starting at age 40 to get a mammography every one or two years to check for breast cancer.
Goal
The aim of a mammogram is to detect breast cancer. Medical experts recommend that mammograms be conducted annually or every other year after age 40 for individuals who were assigned female at birth. Research has shown that regular mammograms can reduce the mortality rate from breast cancer in those aged 40–74.
Mammograms remain the best method of breast cancer screening, but for overall breast health, personal checks are also important. In the case of early-stage breast cancer, mammograms enable a diagnosis before the cancerous cells have spread to any other part of the body, so an early diagnosis can increase the chances of starting therapy sooner to ensure a better prognosis.
Mammography screening
Once you reach your forty’s, your physician most likely will recommend a mammography screening. This kind of test is recommended to patients who have no manifestations of cancer. The purpose of this is early detection and screening for cancer. You can find a tumor as well as microscopic calcium deposits called microcalcifications. These are also known as an early indicator of breast cancer on a mammography screening.
Mammography for diagnosis
If you exhibit any symptoms of breast cancer, your doctor will probably suggest a diagnostic mammography. Finding cancer is the aim of a diagnostic mammography.
Breast cancer symptoms include:
1.A breast lump
2.Breast discomfort or pain
3.The breast’s thicker skin
4.discharge from the breasts
5.A shift in the breast’s dimensions or form
Types of Mammograms
There are two primary varieties of mammograms. According to your age, symptoms, family history, risk factors, and general health, your doctor will suggest a certain kind.
Mammogram in two dimensions
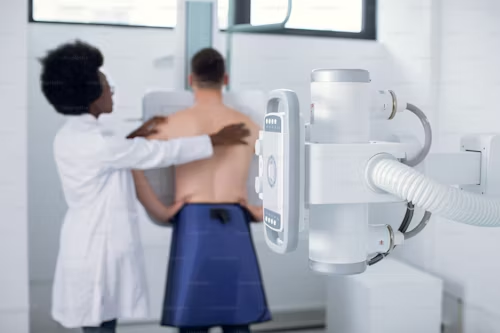
X-ray images of the breast are taken as part of a two-dimensional (2-D) mammography. For screening purposes, your provider will recommend this type of mammography. A technician who specializes in performing mammograms, a mammography technologist will position each of your breasts between two plates during a 2-D mammogram and take photographs to submit to the doctor.
Mammogram three dimensions
As opposed to 2-D mammograms, a three-dimensional mammography, known as a digital breast tomosynthesis, will capture images in much greater detail. In 3-D mammograms, a rotating X-ray machine around your breasts is used so that images can be taken from multiple angles.
In comparison to 2-D mammograms, 3-D mammograms are more sensitive and are able to diagnose more cancer cases.If you have symptoms or signs of breast cancer, your doctor can recommend a 3-D mammography. People with thick breasts also need this type of mammography.
How Does It Work?
A mammography is only a short procedure. During the procedure, a mammography professional will position your breasts correctly and take pictures for you. After finishing, the technician will forward the test results to a radiologist for further evaluation.
Pre-test
You will not need to stop taking any medications or follow a certain diet before your mammogram. You will be asked to complete forms regarding your medical history when you arrive at the medical facility.
If you think you may be pregnant, or even if you simply suspect this, let the medical personnel at the facility know about it. Moreover, you should tell your healthcare professional if you have breast implants as they might cover some tissue in your breast that would be hard to recognize when diagnosing cancer. Lastly, it is necessary to remove all jewelry or metal items prior to beginning the mammography because it might be captured by the X-ray film.
The mammography technician will explain the equipment and the procedure to you when it is time for your scan. You will be asked to put on a front-opening medical gown and undress from the waist up.You will not be given any anesthetic, sedative, or painkillers by your technician before the exam. It will take a few minutes to finish the mammography.
In the course of the test
Your technologist will ask you to step forward in front of the x-ray machine. He/ She will put one of your breasts onto a plastic plate. He/she then positions his/her other plastic plate down on your breast firmly and with plenty of pressure flattens your breast.
In order to prevent movement and improve the quality of images, the breasts have to be flattened during a mammography. Furthermore, flattening the breast ensures that the X-ray photons travel in a shorter distance. This is important because it reduces the radiation exposure you are likely to receive during the scan.
After taking the pictures, the technician will compress the breast using plastic plates to capture a side-view picture. The technician will repeat the procedure with the other breast when you are finished with the first.
It’s essential to know that lots of pressure can be the reason your breasts are being compressed or flattened. Mammograms cause some people a bit of pain, and they can be uncomfortable for most. It takes only a few seconds to complete each picture. You can tell the technologist if you want to take a break while having the test.
Following the Test
You can dress back and go out after the mammography. Because mammography is an outpatient procedure, you can drive yourself home once it is completed.
You can expect to wait from several days to a couple of weeks before your mammogram results are ready. Typically, you will receive a phone call or be called for a follow-up visit in order to discuss the findings of your mammography. Your healthcare provider is likely to recommend additional testing. These may include more mammograms if your mammography results are abnormal.
Hazards and Safety Measures
There are risks of all medical scans and treatments. However, a mammogram is typically considered safe, though not completely risk-free.
Some possible concerns about a mammogram include:
- It is known as a false positive result when a radiologist notices an abnormal area on your mammogram scans but you do not have cancer. You might end up receiving an unnecessary
- second test as a result. Finding out that your results were unusual is also extremely concerning. Those who are younger, have dense breasts, take estrogen supplements, or have had prior breast biopsies are more likely to have false-positive results. Estimated figures suggest that nearly 50% of Americans who have annual breast cancer screenings for a decade or more have at least one false-positive result.
- Overtreatment and overdiagnosis: Mammograms are a very good way to detect cancer. They sometimes discover ductal carcinoma in situ, a condition that affects the cells of the milk ducts in the breast as well as extremely small tumors. These conditions would normally never have threatened your life or caused symptoms. This leads to potentially unnecessary cancer treatment.
- False negative result: When no sign of breast cancer appears in a mammography, it is termed a false negative result. Screening mammography fails to detect breast cancer in an estimated 20% of cases. High breast density may limit tumor detection. Younger persons are also more likely to receive a false negative result.Those who have had previous breast biopsies, those on estrogen supplements, and those whose breasts are thick are considered at risk. Statistics reveal that nearly 50% of Americans who have had annual breast cancer screening tests for more than ten years experience at least one false positive.
- Overtreatment and overdiagnosis: Mammograms are a very good means to detect cancer. They may come across ductal carcinoma in situ, a disorder in which the cells in the milk ducts in your breasts are affected, and an extremely small tumor. In most cases, such disorders would never have even derailed your life and caused symptoms. Thus it leads to unnecessary treatment for cancer.
- A false negative result occurs when there is no evidence of breast cancer, which is confirmed by the mammography. An estimated 20% of cases of breast cancer are missed by screening mammography. Detection of a tumor may also be limited by high breast density. Younger people are also more likely to obtain a false negative result.
- Radiation exposure: A mammogram is an X-ray that takes pictures with tiny amounts of radiation. Repeated X-rays may increase your risk of developing cancer, though it is minimal. A mammography results in a dose of about 0.4 millisieverts (mSv). The general environment in the United States exposes individuals to approximately mSv annually.
How to Prepare for a Breast Exam
It can be intimidating to have a mammogram. It may help to know what to expect. Keep these tips in mind as you prepare for a mammogram:

- Location: An outpatient procedure is a mammogram. Your doctor’s office, private radiology practice, the hospital radiology department, or a breast clinic can offer to schedule a mammogram. A mobile mammography van may also be able to offer one. Food and Drug Administration (FDA) requirements must be met by every mammography facility. Find an FDA approved facility by calling 1-800-4-CANCER (1-800-422-6237).
- Planning: Please note that the week right before your period and your periods are most sensitive days; therefore, your breasts would be bloaty, tender and so planning in advance about the time, date to have the mammogram would best be avoided near this period.
- Clothes: You will be asked to remove your clothes from the waist up during a mammography. Instead of wearing a dress, you may opt for shorts, jeans, or a skirt. Wear perfume or deodorant to your test is not recommended. Also, avoid wearing jewelry.
- Food and drink: You can eat and drink normally before and after your mammography.
- Medication: You can take your usual prescription medications before and after the mammogram.
- Things to bring: Typically, you only need to bring identification and your insurance card to your appointment. The clinic can request you to pay a copay if your insurance does not cover a mammogram or if you are uninsured. Bringing a method of payment may be helpful in some cases.
- Emotional support: Check if your facility is hospitable to visitors by making a call. If you wish to bring a family member, you should know that they are likely to be sent to the waiting room during the mammography procedure.
- Insurance and cost: Most insurance policies cover a mammogram. The Affordable Care Act requires all plans to cover a mammogram every one to two years for women age 40 and older. For patients 40 years and older, Medicare pays for an annual screening mammogram with no deductible.
Findings:
Within a couple of days up to some weeks after having your test, based on the clinic where you went for the mammogram, your result should become available.
The radiologist will write a report after reviewing your photos and send it to your primary healthcare physician. If the results are normal, your provider will contact you by phone, electronic medical record, or letter.
If your results are abnormal, your provider will call you to discuss what is next or schedule a follow-up consultation. They will probably suggest more examinations, such as a breast ultrasound or another mammography.
How to Interpret Your Findings
The radiologist will take care to review the pictures so that any dangerous pattern could be seen for proper interpretation of your mammogram. Radiologists look for white, high-density areas in their picture. They could be malignant. Fatty tissue is translucent and black on an X-ray. For the evaluation of breast tissue, a radiologist can see through it. Dense breast tissue is less possible to differentiate from malignant tissue on a mammography as it has less fat in it and appears white. Be sure to tell your mammography technician while getting the test done if you have been told beforehand that your breasts contain a lot of dense tissue.
One of the above outcomes will be given to you when your doctor transmits the report with the results to you.
- Normal outcome: A normal result indicates that the radiologist did not find any suspicious or malignant regions.
- An abnormal result means that the radiologist saw abnormalities, for example, cancerous lesions. The following measures such as a follow-up mammography will be discussed with you by your doctor.
- Inconclusive result: It becomes inconclusive if your radiologist could not point to any regions of interest for your mammography images. So, you and your practitioner will discuss further follow up, which can either mean another imaging test, in the form of a mammography.
